Do You Suffer From Gastric Varices?
Do you or someone you care about suffer from the painful and potentially life-threatening symptoms of gastric varices? Feeling overwhelmed by the complexity of treatment options and unsure where to turn for help? You’re not alone. Gastric varices affect thousands worldwide, causing debilitating symptoms like vomiting blood, abdominal pain, and fatigue. But there’s hope. With advances in medical technology and minimally invasive procedures, it’s now possible to effectively manage and treat gastric varices. On this page, we’ll guide you through the latest treatment options, including Retrograde Transvenous Obliteration (RTO) and Transjugular Intrahepatic Portosystemic Shunt (TIPS).
What are Gastric Varices?
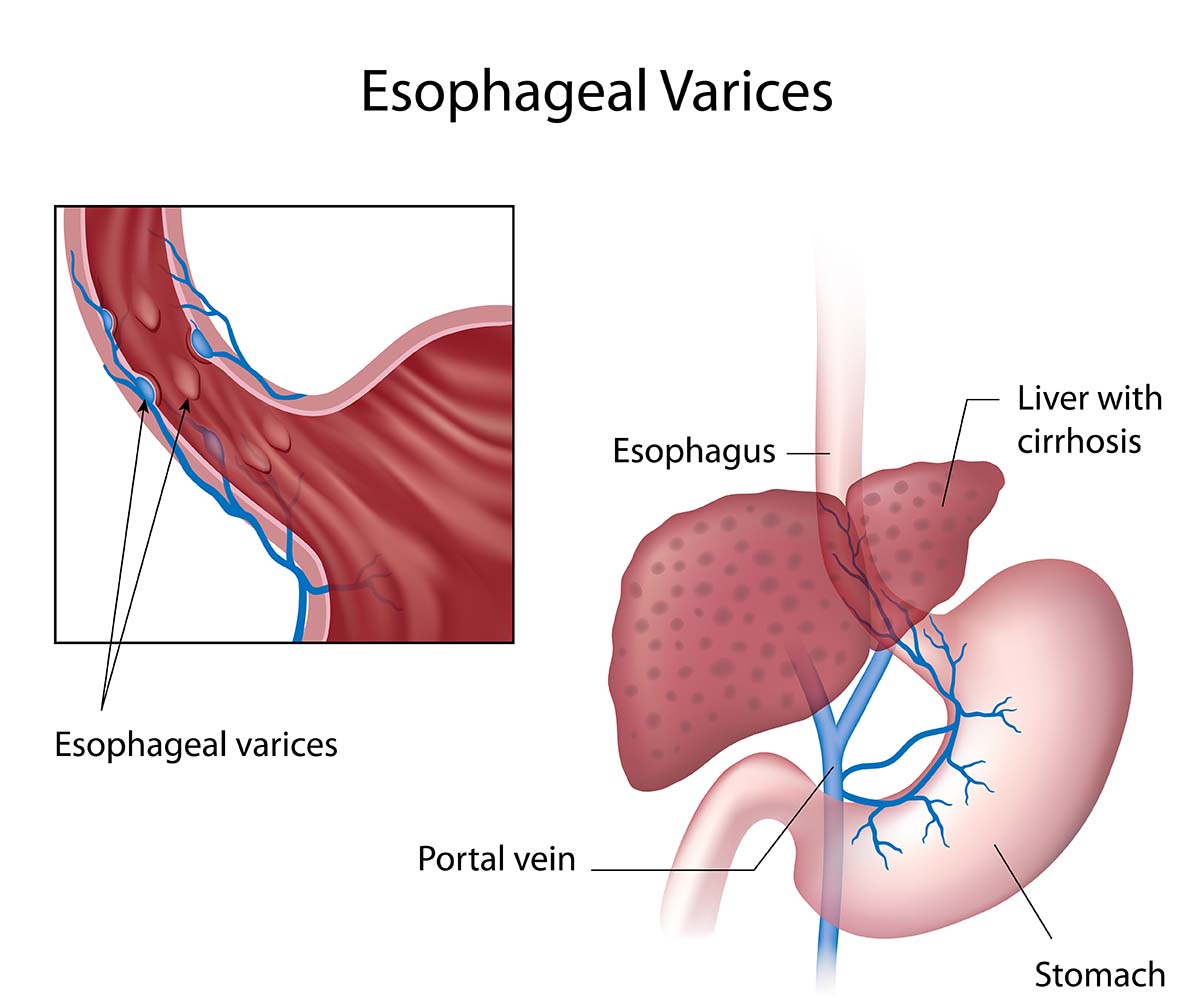
Think of varices as balloons inside your body that can get too big and burst. When this happens in your stomach, it’s called gastric variceal bleeding. It’s a serious condition often caused by high blood pressure in the liver, which acts like a filter to keep your body healthy. Fortunately, there are treatments like BRTO, CARTO, and PARTO that can address the problem without major surgery.
What Causes Gastric Varices?
Gastric varices occur when increased blood pressure in the liver causes blood vessels in the stomach to become enlarged and fragile. This pressure can result from liver cirrhosis, blood clots, or other conditions affecting blood flow to the liver.
Gastric varices occur when increased blood pressure in the liver causes blood vessels in the stomach to become enlarged and fragile. This pressure can result from liver cirrhosis, blood clots, or other conditions affecting blood flow to the liver.
Symptoms of Gastric Varices
Look out for these symptoms of gastric varices:
- Vomiting blood or passing black tarry stools
- Abdominal pain or tenderness
- Nausea and vomiting
- Fatigue and weakness
- Pale or cool skin
How Gastric Varices is Diagnosed
When it comes to diagnosing gastric varices, doctors have several reliable methods to ensure they get it right:
- Endoscopy: This is often the go-to method. It involves using a flexible tube with a tiny camera to look inside your stomach and esophagus, checking for those troublesome enlarged veins.
- Imaging Studies: CT scans and MRIs are great for getting detailed pictures of your liver and the surrounding blood vessels. These images help doctors spot any abnormalities and see how extensive the varices are.
- Blood Tests: These tests can show how well your liver is functioning and if there are any conditions that might be causing increased blood pressure in the liver, which can lead to varices.
By using these diagnostic tools, your healthcare team can accurately identify gastric varices and create a treatment plan that’s just right for you.
Treatment Options for Gastric Varices: TIPS vs. RTO
Retrograde Transvenous Obliteration (RTO) and Transjugular Intrahepatic Portosystemic Shunt (TIPS) are two minimally invasive procedures used to treat gastric varices. While TIPS is the primary treatment, RTO can be an alternative or a complement to TIPS.
What is Transjugular Intrahepatic Portosystemic Shunt (TIPS)?
TIPS involves creating new connections between blood vessels in the liver using a small tube called a shunt. This helps relieve pressure on the dilated vessels, reducing the risk of bleeding.
What is Retrograde Transvenous Obliteration (RTO)?
RTO is a minimally invasive procedure that helps prevent bleeding from enlarged blood vessels in the stomach, known as gastric varices. It involves blocking these vessels to reduce the risk of rupture and bleeding. RTO is often used with or as an alternative to TIPS.
There are several RTO treatment options available:
- Balloon-occluded retrograde transvenous obliteration (BRTO): This involves blocking the enlarged blood vessels in the stomach using a balloon-tipped catheter.
- Coil-assisted retrograde transvenous obliteration (CARTO): This involves using a coil to block the blood flow to the enlarged vessels.
- Plug-assisted retrograde transvenous obliteration (PARTO): This involves using a plug to block the blood flow to the enlarged vessels.
How does the RTO work?
The interventional radiologist will insert a catheter (a thin, flexible tube with a tiny balloon at one end) through a vein in your thigh or neck and guide the catheter to the liver using fluoroscopyfor guidance. The catheter is then directed to the gastrorenal or gastrocaval shunt and the blood flow is blocked.
The interventional radiologist will then perform a venography, which is a type of imaging technique in which X-rays are used to see the vessels clearly. This will allow the interventional radiologist to confirm exactly which vessels need to be treated and if there are any other abnormal or dilated vessels which have not previously been identified. A medication will then be injected into the dilated vessels through the catheter, until they are completely filled.
Another venography will then be performed, to confirm that the blood flow in the shunt has stopped.
Why perform RTO treatment?
You may be advised to undergo this procedure if you are at risk of or already have gastric variceal bleeding and hepatic encephalopathy as well as a gastrorenal shunt. Hepatic encephalopathy refers to the worsening of brain function that is caused by a damaged liver.
Why Choose Southern California Multi-Specialty Center (SCMSC)?
At SCMSC, our team of specialists is dedicated to providing comprehensive care for patients with gastric varices. Our state-of-the-art facilities and minimally invasive procedures ensure that patients receive the best possible treatment with minimal risk and quick recovery times.
If you’re dealing with the symptoms of gastric varices, you don’t have to face it alone. Our compassionate team is here to help. Reach out to us today to schedule an appointment and start your journey to better health. Don’t wait—take the first step towards feeling better now.
The above information is not all inclusive of the risks, alternatives and benefits. It is not meant to be a substitute for informed discussion between you and your doctor, but can act as a starting point for such a discussion. There are complications possible with any medical procedure. Overall, minimally invasive procedures have a lower complication rate than open surgeries.