Fatty Liver Surveillance Program
Monitor Non-Alcoholic Fatty Liver Disease (NAFLD) to identify and intervene if the disease progresses to cancer.
SCMSC’s Fatty Liver Surveillance Program
If you, or a loved one, has been diagnosed with Non-Alcoholic Fatty Liver Disease, you understandably want to monitor the condition closely.
After all, about 10% to 30% of people with this disease have an early stage of Hepatocellular Carcinoma (HCC) which is the third leading cause of cancer death in the United States, and growing yearly.
Southern California Multi-Specialty Center has a new, comprehensive surveillance program for non-alcoholic fatty liver disease to identify and intervene if the disease progresses to hepatocellular cancer.
This program was developed by one of the leading surgeons in the state of California. To find out if you or a loved one qualifies for this program call 818.900.6480 now.
If you want to understand the disease and the surveillance program in greater detail, keep reading. In this article we will discuss the risk factors, progression to cirrhosis, the role of alcohol and genetics, and provide details about the non-alcoholic fatty liver surveillance program.
The Prevalence of HCC in NAFLD
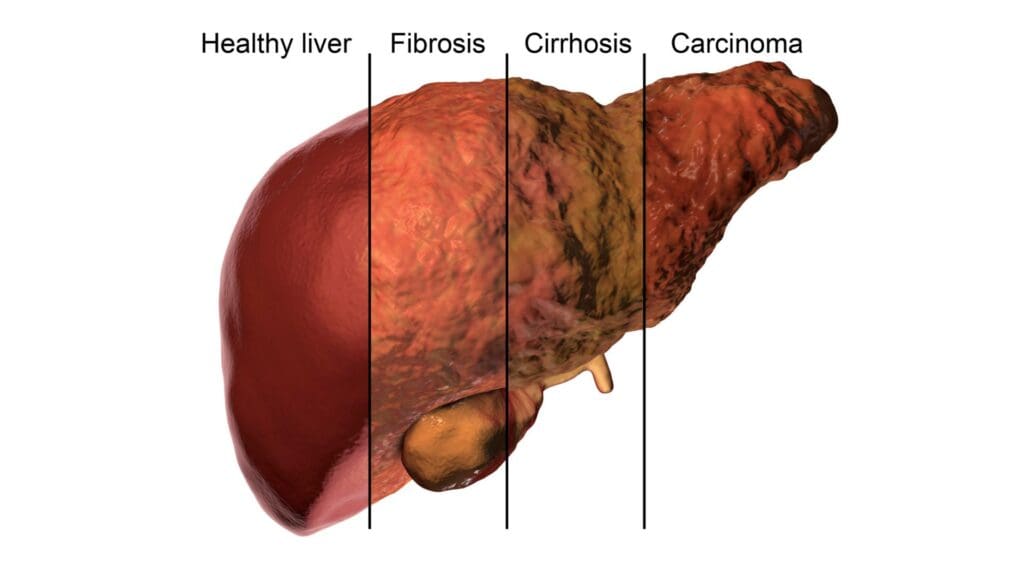
Non-Alcoholic Fatty Liver Disease (NAFLD) impacts more than 25% of the US and global population. About 25% of those individuals progress to nonalcoholic steatohepatitis (NASH). NASH can result in progressive hepatic fibrosis, cirrhosis, and hepatocellular carcinoma (HCC).
About 90% of patients diagnosed with NAFLD have steatosis that is relatively benign but has an overall low mortality rate of 6–8%. However, about 10-30% of those affected have an early stage form of NAFLD non-sympathetic autoimmune disease.
Non-Alcoholic Fatty Liver Disease Q&A
Symptoms of NAFLD may include abdominal swelling (ascites), enlarged blood vessels just beneath the skin’s surface, enlarged spleen, red palms and yellowing of the skin and eyes (jaundice).
What are the risk factors for NAFLD?
- Obesity: Overweight or obese patients have the most significant risk factor for NAFLD. The excess body fat can lead to the accumulation of fat in the liver.
- Type 2 diabetes: People with type 2 diabetes are at higher risk of developing NAFLD because of insulin resistance.
- High blood pressure: High blood pressure can damage the liver and increase the risk of NAFLD.
- High cholesterol and triglycerides: Elevated levels of cholesterol and triglycerides in the blood can lead to the development of NAFLD.
- Metabolic syndrome: This is a cluster of conditions that include obesity, high blood pressure, high blood sugar, and high cholesterol levels. People with metabolic risk factors are at higher risk of developing NAFLD.
- Sleep apnea: People with sleep apnea, a condition where breathing repeatedly stops and starts during sleep, are at higher risk of developing NAFLD.
- Sedentary lifestyle: Lack of physical activity can increase the risk of NAFLD.
- Age: NAFLD is more common in people over 50 years old.
- Genetics: Certain genetic mutations can increase the risk of NAFLD.
It is important to note that not everyone with these risk factors will develop NAFLD, and some people without any risk factors may still develop the condition.
What are the risk factors for Cirrhosis?
there are several risk factors that have been identified:
- Alcohol abuse: Heavy and prolonged alcohol consumption is the most common cause of cirrhosis.
- Chronic viral hepatitis: Chronic hepatitis B or C can cause inflammation and damage to the liver, which can lead to cirrhosis.
- Non-alcoholic fatty liver disease: Accumulation of fat in the liver, known as non-alcoholic fatty liver disease (NAFLD), can progress to cirrhosis in some cases.
- Autoimmune hepatitis: An autoimmune disorder where the immune system attacks liver cells, leading to inflammation and damage, can cause cirrhosis.
- Primary biliary cholangitis: A disease that causes inflammation and damage to the small bile ducts in the liver, leading to cirrhosis.
- Primary sclerosing cholangitis: A disease that causes inflammation and scarring of the bile ducts in the liver, leading to cirrhosis.
- Hemochromatosis: A genetic disorder where the body accumulates too much iron, which can damage the liver and lead to cirrhosis.
- Wilson’s disease: A rare genetic disorder where the body accumulates too much copper, which can damage the liver and lead to cirrhosis.
- Nonalcoholic steatohepatitis (NASH): A severe form of non-alcoholic fatty liver disease that involves inflammation and damage to liver cells, leading to cirrhosis.
- Chronic exposure to toxins: Exposure to certain chemicals, such as those found in pesticides, can lead to cirrhosis.
It is important to note that not everyone with these risk factors will develop cirrhosis, and some people without any risk factors may still develop the condition. Early diagnosis and management of these risk factors can help prevent or delay the development of cirrhosis.
What Is the definition of alcohol abuse?
According to the Centers for Disease Control and Prevention (CDC), heavy alcohol consumption is defined as consuming more than 14 drinks per week for men and more than 7 drinks per week for women. Prolonged alcohol consumption refers to drinking at this level for an extended period of time, typically for years.
It is important to note that heavy and prolonged alcohol consumption can vary based on factors such as body mass index, age, and health status. Additionally, even lower levels of alcohol consumption can contribute to the development of liver diseases and other health problems over time, especially in people who are susceptible to the effects of alcohol.
Timing: NAFLD to Cirrhosis
An old school of thought was that progression from the early stage of patients with NAFLD to cirrhosis took decades, but recent studies have shown that some people this chronic liver disease progresses rapidly within 2 years. However, research has also shown that there is reversibility, which is why Dr. Bobby Eghbalieh created this fatty liver disease surveillance program.
Risk of non-alcoholic fatty liver disease increases with obesity, type 2 diabetes, high blood pressure, high cholesterol, metabolic syndrome, sleep apnea and a sedentary lifestyle.
What is this new surveillance program?
As with other chronic noncirrhotic liver diseases, follow-up of NAFLD (Non-Alcoholic Fatty Liver Disease) patients should consist of monitoring biochemical, metabolic and body weight parameters every 6 months and performing abdominal ultrasound every 6 months.
At SCMSC enrollment in the inclusive surveillance program consists of the following:
- Ultrasound every 6 months for 2 years and then yearly after that
- Fasting bloodwork every 6 months for 2 years and then yearly after that
- Custom nutrition plan based on your specific dietary needs from our in-house specialty dietician
- Lifestyle modification plan
- Proprietary supplementation plan customized for each patient to promote liver regeneration and reversal of disease
Make an Appointment
You are not alone in this health journey. The SCMSC team in LA is always here, blending professional expertise with a touch of human understanding.
To schedule an evaluation with Dr. Eghbalieh or Dr. Young at Southern California Multi-Specialty Center, call 818-900-6480.
Make an appointment at SCMSC
We look forward to welcoming you