What are minimally invasive endovascular procedures, and why might they be a suitable option for treating vascular conditions? These advanced techniques leverage small incisions and imaging guidance, aiming to minimize patient downtime and postoperative discomfort. In this comprehensive guide, we’ll navigate the specifics of the procedure, potential benefits, the conditions they can treat, and what you should know about recovery and risks involved.
Key Takeaways
- Minimally invasive endovascular surgery provides a less traumatic alternative to traditional open surgery, offering benefits such as reduced blood loss, decreased infection risk, and quicker recovery times.
- Endovascular procedures address a vast range of vascular diseases, including aneurysms and peripheral artery disease, with specific techniques like thrombolysis and endovenous laser therapy tailored to each condition.
- The field of endovascular surgery is continually advancing with innovative techniques such as FEVAR and the use of endoanchors, improving patient outcomes for complex vascular conditions.

Understanding Minimally Invasive Endovascular Surgery
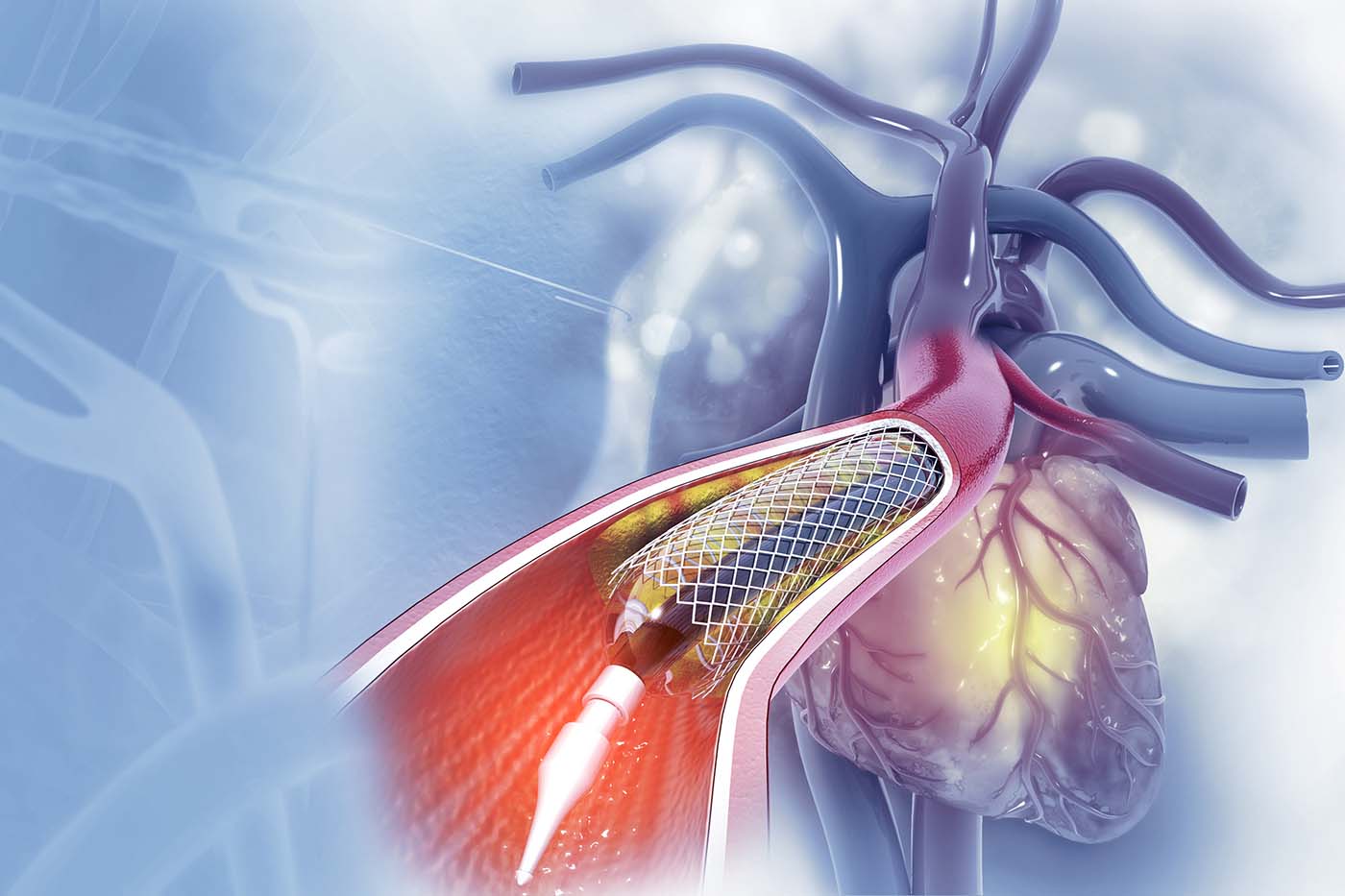
Endovascular surgery might sound like a mouthful, but its concept is simpler than you think. This surgical approach is an alternative way to repair conditions that affect the movement of blood throughout the body. Imagine a team of mini doctors, armed with catheters, accessing your arteries and veins for diagnosis and treatment. Instead of making large incisions, they repair blood vessels and remove clots through small punctures. This minimally invasive approach results in less blood loss and quicker recovery compared to open surgery.
Picture it this way: a small incision is made, much like a door opening. This gives access to a primary blood vessel. Next, a catheter, a thin tube, is introduced subcutaneously (under the skin). This catheter then serves as a pathway to reach the problematic areas. It’s like having a private, internal highway to deliver treatment right where it’s needed.

The Spectrum of Conditions Addressed by Endovascular Procedures
- Aneurysms
- Atherosclerosis
- Carotid artery disease
- Deep vein thrombosis
- Peripheral artery disease
To put it into perspective, peripheral artery disease alone affects eight to 12 million Americans. Further, about 200,000 individuals in the United States are diagnosed with abdominal aortic aneurysms each year. Quite astonishing, isn’t it?
But that’s not all. There are specific endovascular procedures tailored to treat different vascular conditions. For deep vein thrombosis, treatments involve thrombolysis, the application of anticoagulant medications, and the insertion of inferior vena cava filters. Moreover, varicose veins, those unsightly twisted, enlarged veins, can be treated with minimally invasive endovascular treatments such as sclerotherapy, radiofrequency ablation, and endovenous laser therapy. The versatility of endovascular treatments is truly remarkable, allowing for personalized care for a wide spectrum of conditions.

The Procedure: How Minimally Invasive Endovascular Surgery Works
Let’s take a deeper dive into how minimally invasive endovascular surgery works. As we have mentioned earlier, the procedure typically involves the following steps:
- A small incision is made to access a primary blood vessel.
- A catheter is inserted subcutaneously, serving as a pathway to the problem area.
- The catheter acts like a secret tunnel leading directly to the villain’s lair, allowing the surgical team to swoop in and save the day.
But what guides the team through this tunnel? This is where technology comes into play. Advanced imaging technologies such as cone-beam computed tomography (CT) play a significant role in these procedures. In fact, they are increasingly being utilized in fenestrated and branched endovascular procedures to assess the stent architecture and facilitate successful outcomes. These imaging technologies act as the navigation system, guiding the surgical team to ensure accurate and precise treatment.
This combination of a minimally invasive procedure and advanced technology results in an approach that is:
- Less traumatic than traditional open surgery, including minimally invasive surgery
- Reduces blood loss
- Decreases the risk of infection
- Leads to a quicker recovery
- Offers the benefits of minimally invasive procedures
It’s a win-win situation for both the surgical team and the patient.
Preparing for Your Procedure: Steps to Take Before Endovascular Surgery
Before you step into the surgical suite, there are some necessary preparations to be made. The first step involves providing a full medical history, undergoing a physical examination, and completing diagnostic tests including blood tests. Think of it as laying down the groundwork. This information is crucial for your healthcare provider to understand your health status and plan the procedure accordingly.
Next comes fasting. You need to:
- Fast for at least eight hours before the procedure, typically starting after midnight.
- Discuss any potential allergies or medications with your physician. Whether you are allergic to medications, latex, iodine, tape, contrast dyes, or anesthetic agents, your healthcare provider needs to know.
- Report all medications you are taking, including prescribed, over-the-counter, and herbal supplements. This ensures that your healthcare provider can make necessary adjustments to ensure your safety during the procedure.
Recovery Insights: What to Expect After Endovascular Surgery
Once the procedure is completed, what’s next? The typical recovery period after minimally invasive endovascular surgery is usually about two weeks. Here’s what you can expect during the recovery process:
- Immediately following surgery, your vital signs are closely monitored.
- You are required to lie flat for several hours to prevent bleeding.
- You are allowed to walk and progressively increase activities.
- Eventually, you can return to a normal diet as tolerated.
Upon returning home, patients need to:
- Keep the surgical area clean and dry
- Follow your provider’s instructions on activity levels and bathing
- Avoid driving until cleared by a physician
- Manage pain with medication as recommended
- Have sutures or staples removed at a follow-up visit unless done prior to hospital discharge
Your healthcare provider is your ally during this recovery period, so don’t hesitate to reach out if you have questions or concerns.
Potential Complications and How They’re Managed
While minimally invasive endovascular surgeries revolutionize the treatment of vascular conditions, it’s essential to understand that no surgical procedure is without its potential risks. Complications during these surgeries are rare, but may include:
- Infection
- Leaking of blood
- Blockage of blood flow
- Fever
- Burst artery
- Kidney injury
However, rest assured that your healthcare provider is well equipped to manage these complications if they arise.
The incidence of complications such as vein tearing or rupture is generally low. However, if complications do arise, management may range from symptomatic treatment to more serious interventions such as graft occlusion. After surgery, patient monitoring is conducted in intensive care or post-anesthesia units, where vital signs such as blood pressure and oxygen levels are closely watched. Patients are advised to promptly report any post-surgery symptoms including:
- fever
- chills
- increased pain
- issues at the incision site
This is to ensure timely management of any arising complications.
Innovative Techniques in Endovascular Surgery
The field of endovascular surgery is one that continuously evolves, thanks to innovative techniques such as parallel grafting and hybrid operating rooms. These innovations have expanded surgical options by allowing a combination of open and endovascular techniques to be used during vascular surgeries. One such procedure that can be performed in these hybrid operating rooms is Fenestrated Endovascular Aortic Aneurysm Repair (FEVAR). This facilitates treatment for complex aortic aneurysm cases.
Furthermore, clinical research like the PROTAGORAS 2.0 study is working towards standardizing ChEVAR procedures by developing new planning and sizing rules for improved patient outcomes. Use of endoanchors in Endosuture Aneurysm Repair (ESAR) has been associated with reduced complication and reintervention rates for patients with wide-neck aortic aneurysms. These advancements are pushing the boundaries of what’s possible in the field of endovascular surgery, leading to safer procedures and improved patient outcomes.

The Role of Interventional Radiology in Vascular Health
Interventional radiology plays a vital role in maintaining vascular health. It is a subspecialty centered on minimally invasive image-guided procedures to diagnose and treat diseases. Through its evolution, it has replaced many traditional surgeries, offering benefits such as reduced risks and shorter recovery times. Interventional radiologists undergo an additional six to seven years of training beyond medical school, including a focused fellowship, underscoring their high level of expertise in conducting endovascular procedures.
Advanced imaging technologies such as:
- ultrasounds
- CT scans
- MRI
- fluoroscopy
are pivotal in the diagnosis of venous diseases and the guidance of precise interventional procedures. These imaging technologies enable minimally invasive approaches, creating a roadmap for the surgical team to navigate through the body’s intricate network of blood vessels. Furthermore, interventional radiologists are equipped with the skills and tools to promptly manage any complications that might arise during endovascular surgeries, ensuring patient safety and positive outcomes.
Choosing the Right Vascular Center for Your Treatment
When it comes to your health, making the right choice is essential. The right choice for a vascular center is one with:
-
Surgeons who specialize in your condition, providing optimal care and treatment outcomes
-
Comprehensive diagnostic and treatment services in a single location, enhancing your experience and providing convenience
-
A team of experts who are dedicated to your care and well-being
Choosing a vascular center that meets these criteria can ensure that you receive the best possible care for your condition.
Furthermore, high-quality vascular centers:
-
Track and uphold outcomes that meet or exceed established care standards. This reflects their commitment to excellence and trustworthy care.
-
Utilize a team-based approach to ensure a more effective and tailored plan for your treatment.
-
Offer same-day returns home and quicker recovery through facilities with ambulatory units.

Southern California Multi-Specialty Center
Among the frontrunners in the field of minimally invasive endovascular procedures is the Southern California Multi-Specialty Center (SCMSC). SCMSC stands out as one of the most experienced procedural centers in California, providing specialized services in:
-
General surgery
-
Vascular surgery
-
Interventional radiology
-
Podiatry
At SCMSC, you are in good hands with Drs. Eghbalieh and Abi-Chaker, who have years of extensive training focused on their chosen specialty of vascular surgery. This level of expertise ensures that no other specialty is better trained and more equipped to diagnose and treat vascular disorders than the vascular surgeons at SCMSC.

Maintaining Vascular Health Post-Surgery
Following your treatment to treat vascular disease, maintaining your vascular health is essential to prevent issues such as blood clot formation. This involves:
-
A healthy lifestyle, including regular exercise and a balanced diet
-
Regular follow-up appointments to monitor your progress and catch any potential issues early
-
Adhering strictly to any prescribed medications to prevent blood clots and manage health conditions
Smoking cessation is also strongly encouraged. Not only does it enhance your chances of recovery, but it significantly improves your overall vascular health. Your journey to good health doesn’t end with the surgery; it’s a lifelong commitment to maintaining a healthy lifestyle.
Contact SCMSC now for an appointment or for more information.
If you’re ready to take the first step towards better vascular health, or simply want to learn more about minimally invasive endovascular procedures, don’t hesitate to contact SCMSC. With our team of experienced doctors who offer personalized care and employ minimally invasive techniques, we’re committed to your health and wellbeing. You can schedule an appointment at any of our locations throughout the San Fernando Valley at convenient hours to suit your needs.
Join us at SCMSC, where we integrate a comprehensive health perspective, aiming to improve your overall wellbeing along with addressing specific medical conditions.
Summary
In the ever-evolving field of medicine, minimally invasive endovascular procedures have emerged as a game-changer in the treatment of vascular conditions. Offering a less invasive alternative to traditional surgery, these procedures enable quicker recovery times, reduced blood loss, and less trauma to the body. From the wide range of conditions that can be addressed, the detailed procedure, preparation, and recovery process, potential complications, to the innovative techniques and the crucial role of interventional radiology, we’ve delved into the key aspects of these revolutionary procedures.
Choosing a reputable vascular center like the Southern California Multi-Specialty Center (SCMSC) ensures that you have a team of experienced vascular surgeons at your service. As we conclude, remember that maintaining your vascular health is a lifelong commitment that goes beyond the surgery itself. So, why wait? Contact SCMSC today and take the first step towards better vascular health. Your journey to better health starts here.
Frequently Asked Questions
What are minimally invasive endovascular procedures?
Minimally invasive endovascular procedures are a less invasive alternative to traditional surgery, using catheters to access arteries and veins for diagnosis and treatment, resulting in less blood loss and quicker recovery.
What conditions can be treated with endovascular procedures?
Endovascular procedures can effectively treat a variety of vascular conditions such as aneurysms, atherosclerosis, carotid artery disease, deep vein thrombosis, and peripheral artery disease. These procedures offer a comprehensive approach to managing various vascular diseases.
How do I prepare for an endovascular procedure?
To prepare for an endovascular procedure, make sure to provide your full medical history, undergo diagnostic tests, fast for at least eight hours before the procedure, and discuss any potential allergies or medications with your physician. This will help ensure a smooth and successful procedure.
What is the recovery process like after endovascular surgery?
After minimally invasive endovascular surgery, the typical recovery period is about two weeks. Patients should follow their provider’s instructions on activity levels and bathing, and gradually increase activities and return to a normal diet as tolerated.
What is the role of interventional radiology in vascular health?
Interventional radiology plays a crucial role in vascular health by providing minimally invasive image-guided procedures to diagnose and treat diseases, offering benefits such as reduced risks and shorter recovery times.
About the Author
Sammy Eghbalieh, MD, FACS, FSVS, RPVI
Dr. Sammy Eghbalieh of Vascular and Endovascular Surgery; Director of Vascular Imaging, Southern California Multi-Specialty Center (SCMSC). Dr. Sammy Eghbalieh is a board-certified expert in vascular, endovascular, and minimally invasive surgery. His expertise encompasses a wide range of venous and arterial diseases, and he is dedicated to providing advanced care to his patients at SCMSC. He is a Board-Certified in Vascular and Endovascular Surgery; fellow of the American College of Surgeons (FACS); a diplomate of the Society for Vascular Surgery (DFSVS); and a Registered Physician in Vascular Interpretation (RPVI).
Learn more about Southern California Multi-Specialty Center. Read our editorial policy.