Reliable Dialysis Access: Your Lifeline to Effective Treatment
When kidney function declines to the point where dialysis becomes necessary, establishing reliable vascular access isn’t just a medical formality – it’s the lifeline that makes treatment possible. At Southern California Multi-Specialty Center in Los Angeles, our vascular surgeons specialize in creating and maintaining dialysis access for patients with end stage renal disease, including advanced solutions like the HeRO Graft for those facing complex venous challenges.
The difference between struggling through dialysis and receiving effective treatment often comes down to one factor: the quality of your vascular access. A properly functioning AV fistula or graft delivers adequate blood flow for hemodialysis treatments, reduces infection risk compared to catheters, and provides the long term dialysis access your care team needs to keep you healthy.
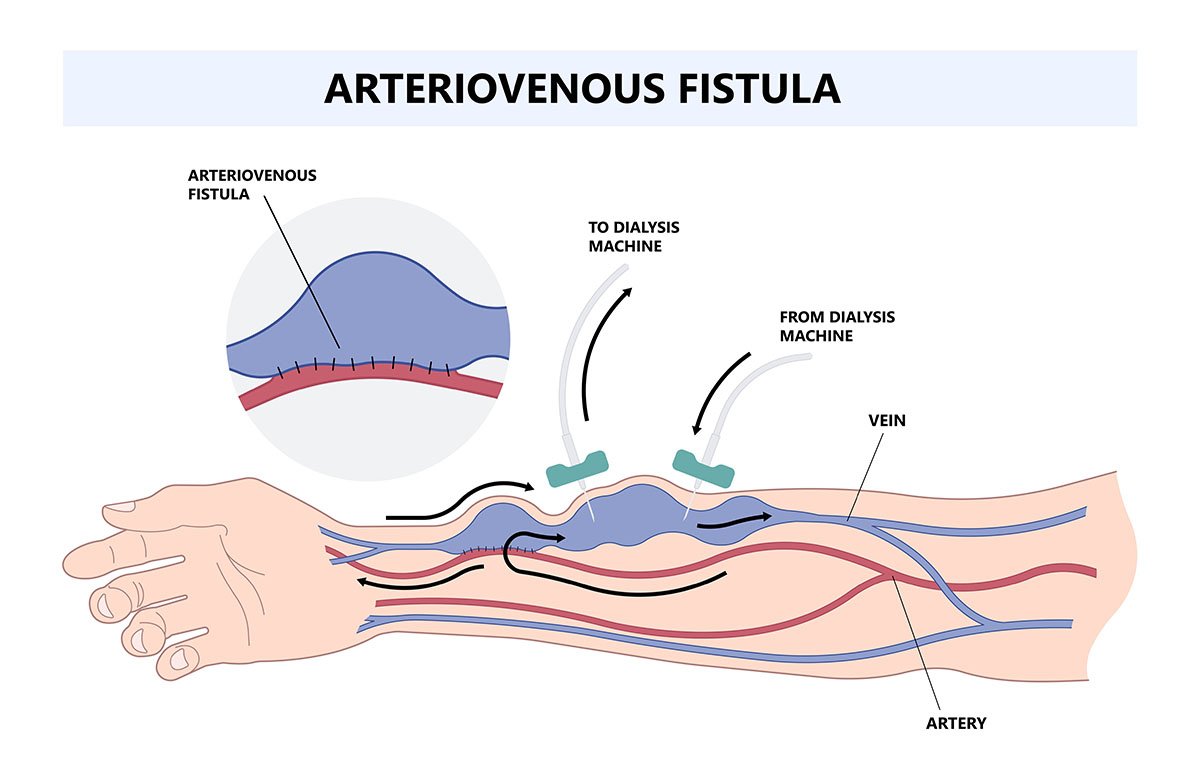
What Is an Arteriovenous Fistula?
An arteriovenous fistula is a surgical connection between an artery and a vein, typically created in the arm to establish dialysis access. This connection allows blood to flow directly from the artery into the vein, causing the vein to enlarge and strengthen over several weeks. Once matured, this access site can be used repeatedly for hemodialysis treatments—providing the high blood flow rates needed to filter your blood effectively.
The surgical procedure involves making a small incision in your arm and connecting the radial artery or brachial artery to a nearby vein, such as the cephalic vein or basilic vein. This creates permanent vascular access that can last years with proper care, far outlasting temporary access options like dialysis catheters.
Types of Dialysis Access: Understanding Your Options
Patients with chronic kidney disease requiring hemodialysis access have three primary options, each with distinct advantages depending on your vascular anatomy and medical history.
AV Fistula Creation
The preferred choice for most patients, an AV fistula uses your own blood vessels to create a direct connection. Common types include the radiocephalic fistula (radial artery to cephalic vein at the wrist), brachiocephalic fistula (brachial artery to cephalic vein in the upper arm), and transposed brachiobasilic fistula (basilic vein surgically repositioned). These require one to two hours in the operating room and typically mature within several weeks before they can support dialysis therapy.
Arteriovenous Graft
When your veins aren’t suitable for fistula creation, AV grafts provide an alternative. This surgical procedure uses synthetic material—a thin plastic tube that acts as a bridge between an artery and a vein. AV graft surgery creates access that can often be used sooner than a fistula, though grafts typically have a shorter lifespan and require more frequent monitoring for blood clot formation.
Dialysis Catheters
Reserved for temporary access or emergency situations, catheters are thin plastic tubes inserted into large veins in your neck or chest. While they allow immediate dialysis, catheters carry higher infection rates and don’t provide the blood flow quality achieved with fistulas or grafts. They’re never the goal for long term dialysis—they’re a bridge until permanent access can be established.
HeRO Graft: Advanced Solution for Complex Dialysis Access
Some patients face a frustrating reality: traditional AV fistula or graft options have been exhausted due to central venous stenosis – blockages in the large veins leading to your heart. For years, this meant permanent dependence on catheters with their associated infection risks and treatment limitations.
The Hemodialysis Reliable Outflow (HeRO) Graft changes this equation. This specialized system consists of two components: a standard arteriovenous graft in your arm connected to a small wire mesh tube (nitinol component) that’s threaded through the blocked veins directly into your heart. The HeRO Graft bypasses venous obstructions that would make traditional fistula or graft placement impossible.
Clinical data shows HeRO Grafts maintain patency rates comparable to conventional AV grafts – up to 87% at two years – while reducing infection risk by 69% compared to catheter dependence. For patients who’ve been told they have “no more access options,” the HeRO Graft represents a path back to effective dialysis without the complications of permanent catheter use.
When Traditional Access Fails: Who Needs Advanced Solutions
HeRO Graft placement isn’t a first-line option—it’s the solution when standard approaches won’t work. Our vascular surgeons evaluate you for HeRO Graft if you meet specific criteria: all traditional upper extremity access options have been exhausted, you have central venous occlusion confirmed by imaging, you maintain adequate blood pressure to support the graft, and your kidney failure requires extended hemodialysis access (typically more than one year before potential transplant).
The multidisciplinary team at SCMSC collaborates to determine whether HeRO Graft placement offers the best path forward for your individual situation.
The AV Fistula Surgery Experience at SCMSC
Understanding what happens during AV fistula creation helps reduce anxiety and prepares you for recovery. Our process prioritizes both immediate success and long-term access durability.
Before surgery, you’ll undergo a physical examination and vascular mapping – typically an outpatient procedure using ultrasound to evaluate your blood vessels. We assess artery and vein size, blood flow patterns, and identify the optimal location for surgical connection. Most patients receive their fistula in the non dominant arm when possible, though vascular anatomy sometimes dictates otherwise.
The surgical procedure itself is performed on an outpatient basis under local anesthesia, though some cases may use general anesthesia depending on complexity and patient preference. Your vascular surgeon makes a surgical incision, identifies the appropriate artery and a vein, then creates the connection that will allow more blood to flow through the vein. The incision is closed, a sterile dressing is applied, and you’re monitored briefly before going home the same day.
Most AV fistula surgery takes one to two hours. You’ll feel the characteristic “thrill” – a vibration from blood flow – at the access site immediately after creation, confirming the connection is functioning.
Recovery and Fistula Maturation: What to Expect After AV Fistula Surgery
The recovery time for AV fistula surgery varies by individual, but most patients resume normal activities within days. The real timeline, however, is fistula maturation – the process where increased blood flow causes the vein to enlarge and its walls to thicken enough to withstand repeated needle insertions.
During the first several weeks, your access arm will show progressive changes. The vein becomes more prominent, you’ll feel the thrill continuously, and the vessel strengthens. This maturation period typically requires six to twelve weeks before your dialysis fistula is ready for use, though some fistulas mature faster while others need additional time or interventional support.
Your care team will provide specific instructions for protecting your new fistula: avoid blood pressure measurements on the affected arm, don’t allow blood drawn from the fistula, keep the area clean, and immediately report any concerning symptoms. Daily checks of the thrill – that buzzing sensation confirming blood flow – become part of your routine. If the thrill disappears or changes, this should be promptly reported as it may signal stenosis or blood clot formation requiring intervention.
Common Complications and When to Seek Help
Even well-created fistulas can develop problems. Stenosis, narrowing of blood vessels at the surgical connection or in the venous system, is the most common issue, often treatable through minimally invasive procedure like balloon angioplasty. Some patients develop steal syndrome, where the fistula diverts too much blood from your hand, causing pain or coldness that may require surgical revision.
Infection remains a concern with any vascular access, though fistulas have far fewer problems than catheters. Signs warranting immediate attention include fever, redness, warmth, or drainage at the access site, sudden swelling in your arm, loss of the thrill sensation, or increasing pain. Early intervention often prevents access loss, so don’t hesitate to contact your vascular surgeon if something seems wrong.
Blood clot formation (thrombosis) can suddenly block your dialysis fistula. This requires urgent evaluation and often thrombectomy to restore blood flow before permanent damage occurs. The sooner we intervene, the better the chance of salvaging your access.
AV Grafts vs. Fistulas: Understanding the Trade-offs
While AV fistula creation remains the gold standard for permanent vascular access, AV grafts serve an important role when fistula placement isn’t possible. Grafts use synthetic material to bridge artery directly to vein, creating functional access faster than fistulas mature.
The surgical procedure for AV graft placement is similar to fistula creation but involves implanting the graft material – usually polytetrafluoroethylene (PTFE). These can typically be used for hemodialysis treatments within two to four weeks rather than the longer fistula maturation time.
However, AV grafts have trade-offs. They’re more prone to stenosis and thrombosis than fistulas, requiring more frequent monitoring and intervention to maintain patency. Infection rates are higher than fistulas though still lower than catheters. Life expectancy for grafts averages three to five years compared to potentially decades for well-functioning fistulas.
For patients with small veins, previous access failures, or medical conditions affecting vessel quality, grafts provide reliable dialysis access when fistulas aren’t feasible.
Dialysis Access Maintenance: Protecting Your Lifeline
Creating your fistula or graft is just the beginning—maintaining it requires partnership between you and your care team. Regular monitoring catches problems early, when they’re most treatable. Your dialysis center tracks access flow rates, watches for prolonged bleeding after needle removal, and reports concerning trends to your vascular surgeon.
You play the critical role in daily surveillance. Check your thrill every morning and evening. Note any changes in how your access site looks or feels. Avoid tight clothing or jewelry on your access arm. Keep blood pressure cuffs, IVs, and blood draws away from your fistula. These simple practices dramatically reduce complications and extend access lifespan.
When problems arise, interventional radiologists at SCMSC can often address them through minimally invasive procedures rather than surgery. Vascular stenting opens stenotic segments, balloon angioplasty restores narrowed areas, and thrombectomy clears clots – often performed on an outpatient basis under local anesthetic with faster recovery than open surgical revision.
Beyond Hemodialysis: Understanding All Kidney Failure Treatment Options
While our focus is creating optimal hemodialysis access, understanding the full spectrum of kidney failure treatments helps you make informed decisions with your dialysis team. Peritoneal dialysis uses your abdominal cavity to filter blood through a catheter placed in your belly, avoiding the need for vascular access entirely. This home-based option suits some patients’ lifestyles and medical situations.
Kidney transplantation remains the ultimate goal when possible, offering the best life expectancy and quality of life for patients with end stage renal disease. Even while on dialysis, maintaining your vascular access properly keeps you healthy enough to qualify for transplant when an organ becomes available.
The SCMSC Advantage: Multidisciplinary Dialysis Access Care
Establishing and maintaining dialysis access demands more than surgical skill – it requires coordinated care across specialties. At SCMSC, our vascular surgeons work alongside dialysis teams to deliver comprehensive access management throughout the San Fernando Valley and greater Los Angeles area.
This collaboration means fewer delays when complications arise, streamlined communication between your surgical and dialysis providers, and access to advanced options like HeRO Graft that many centers can’t offer. When your doctor identifies an access problem, our vascular surgeons can evaluate and intervene quickly.
Our five locations throughout Los Angeles & the San Fernando Valley provide convenient access for patients from Santa Monica, Brentwood, Sherman Oaks, Glendale, Burbank, and surrounding communities throughout Los Angeles County. We understand that managing chronic kidney disease already fills your schedule with dialysis therapy three times weekly – having your surgical care close to home reduces the burden.
Preparing for Your Dialysis Access Consultation
When you meet with our vascular surgeons, come prepared to discuss your complete medical history, previous access attempts if any, your dialysis schedule, and any concerns about the surgical procedure. Bring a list of your current medications including anticoagulants that may need adjustment before surgery.
We’ll perform a physical examination of your arms, feel for artery pulses and examine vein quality, and discuss which type of access – fistula, graft, or HeRO Graft – best fits your vascular anatomy and long-term needs. Many patients benefit from vascular mapping before surgery to plan the optimal approach.
Questions about recovery time, when your access can be used, activity restrictions, and long-term maintenance are all welcome. Understanding the process reduces anxiety and improves outcomes -informed patients are better partners in their own care.
Taking the Next Step
Living with kidney failure requires dialysis access you can depend on. The quality of that access directly impacts your treatment effectiveness, complication rates, and overall quality of life. At SCMSC, our vascular surgeons combine technical expertise with genuine understanding of what you’re facing – because we know your dialysis fistula or graft isn’t just a surgical connection, it’s your lifeline.
Call us at (818) 900-6480 to schedule your dialysis access consultation. Let’s work together to establish reliable vascular access that supports your health for years to come.
Our Vascular & Endovascular Surgeons
It's important to remember not all physicians are trained in advanced vascular and endovascular surgery. It’s a good practice to get multiple opinions and do research on the surgery and the physician.